The identity project - An arts based adaptation of Narrative Therapy Practice.
I am inspired to write about a group that I facilitated this week which combined elements of MIECAT arts therapy procedures with Narrative Therapy outsider witness practice.
Outsider witness practice is well documented in Narrative Therapy literature if you are interested to read more but I give a basic description of it at the end of this post.
In recent years I have been adapting this practice using arts based activities to enrich the already transformative experience.
Yesterday I was asked to run a group therapy session on identity using an art based approach. The clients were a group of people coming to our trauma treatment program and I had not worked with them before. I was told that the group were a bit flat and struggling in the morning and later that day I discovered that the group had previously been having difficulty feeling connected.
Here is a brief outline of the group process I used.
Selecting images
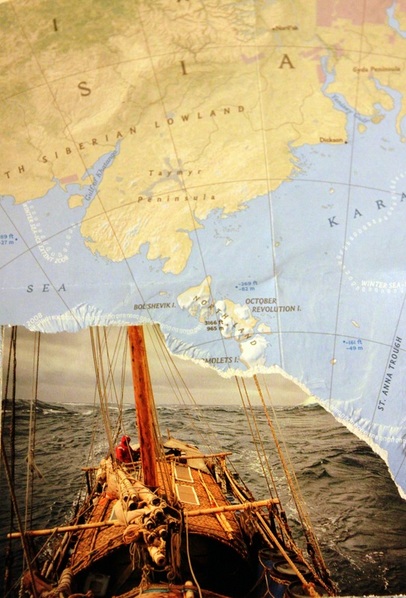
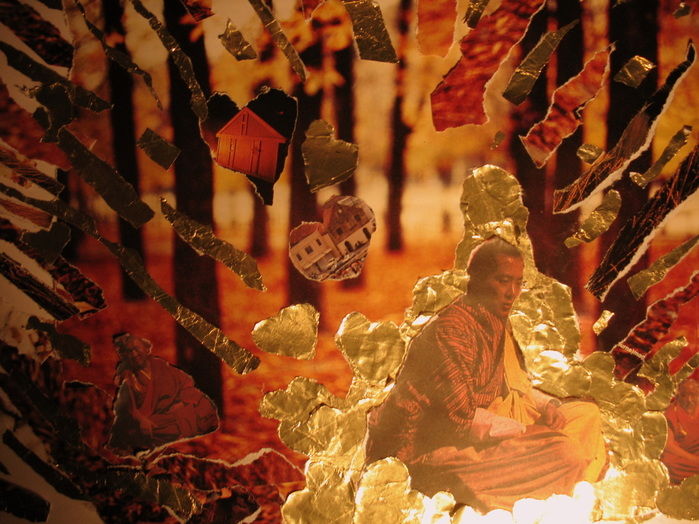
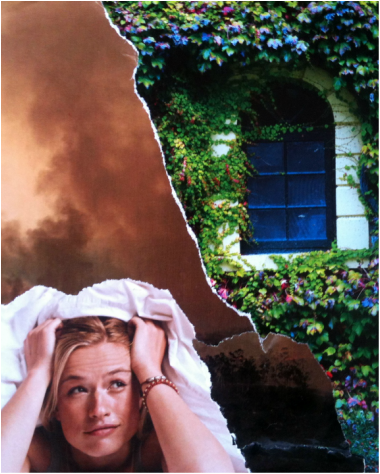
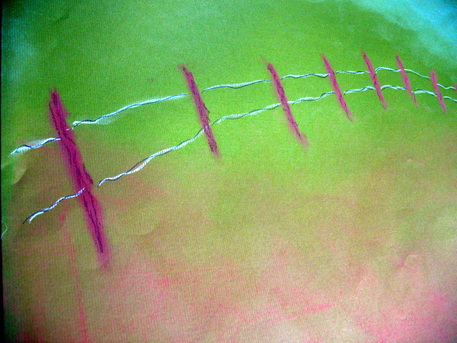
I asked participants to select postcard images (free ones collected from cafes over the years) to describe aspects of themselves which were nothing to do with the experiences or struggles that brought them to our program. Naturally that was difficult as they were feeling overwhelmed by the problems they face, I let them know that even one card that did not relate to problems would be a good job done.
Then I asked them to cluster the cards into groups that seemed to fit together and give each group a name. (This clustering and naming process is a standard MIECAT arts therapy process it helps people make sense of the images and reduce the information held in the cards down to its core message)
The interview process
Group members were instructed to listen to the interview and take down any words or statements that they heard coming out of the interviewees mouth, which stood out to them for any reason. (this is another wonderful MIECAT technique called Key Words. It can be utilised in numerous ways; in this instance, it is serving the purpose of helping the listeners stay focused and engaged and the words collected are essential in our witnessing process)
Facilitator I interviewed each person about the cards they had chosen for about ten minutes. I invited participants to speak of the cards that were not dominated by problems and listened intently for the slightest opportunity to enquire into storylines which would lead the conversation to areas of the participant’s values, skills, knowledge, meaning full relationships etcetera. (In Narrative Therapy these are sometimes called windows of opportunity)
Participants After each interview participants took note of any key words or statements that had strongly resonated with their own experience and then gave all the words they had recorded to the speaker. Participants received these key words with delight.
Key word poetic statements Once everyone had been interviewed I invited participants to pluck out the words and statements that held the most meaning to them from the key words they had been given. (picking out the key words from the key words) they then created poetic statements with the words which they shared with the group. (this is another tried and true MIECAT procedure which again brings the many words down to the essence of what is most important to the individual)
Double listening
Not surprisingly speaking about stories not dominated by problems was very difficult for all the group members on this occasion so I needed to listen intently employing what is sometimes called double listening. Double listening is when you are with one ear hearing the problem dominated story and with the other ear listening for implicit or explicit fragments of preferred identity stories for example values held, skills and knowledge acquired, capabilities developed, relationships of meaning etcetera. By remaining curious, paying close attention and asking skilful questions informed by my narrative therapy training to draw out these alternate stories our conversations took surprising and delightful paths.
Some of the noteworthy things we learned about the group members were: of a powerful and protective sense of wit, a capacity to make life enhancing choices at life’s important junctures, ability to step out of the critical mind whilst play music which might translate into other parts of life, a passion for art and activism, values of living life to its fullest and an emerging capacity for self-compassion.
The power of being witnessed.
Through these conversations the group learned a great deal about each other’s lives which had not previously been explored and participants expressed a new-found appreciation for their group members. The stories we heard in this group stand in stark contrast to the stories of childhood abuse, workplace bullying and injury, emotional suffering, and decreased functioning through which the group had previously known one another. Having your courage, humour, passion, values and capability witnessed by an audience and reflected to you in your own words or through visual image is a powerful tool in reclaiming your sense of self from the effects of traumatic experience or illness.
When the team leader met with the group at the end of the day he described participants as buzzing with excitement when he entered the room and the group reported feeling much more connected with one another than they previously had.
Possibilities to include further art making
There are numerous ways to include more art making into this exercise here are some I have included in the past.
Initial representation can be made in any arts modality.
Visual representation of the essence of the key words can made by interviewee.
Each audience member makes a response in arts modality inspired by the key words they have collected to give to the interviewee.
Audience members make a representation of how the interview might inspire them in their own lives.
A rough outline of Outsider witness process
One person is interviewed by a narrative therapist in front of an audience of one or more.
The audience is then interviewed and asked to reflect on the following.
Some aspect of the interviewees story that caught their attention.
What that aspect of the evoked for them in terms of the interviewees hopes, values ambitions and identity.
How this relates to their own experience.
Where they might have been moved to or how they might be inspired by the experience of listening to the interview.
The original interviewee then speaks about their experience of listening to the audience (the retelling)
If you would like to read more about the use of outsider witness practice in Narrative Therapy I recommend the following article it is readily available on the internet.
Outsider-witness practices: some answers to commonly asked questions”
Maggie Carey & Shona Russell
Outsider witness practice is well documented in Narrative Therapy literature if you are interested to read more but I give a basic description of it at the end of this post.
In recent years I have been adapting this practice using arts based activities to enrich the already transformative experience.
Yesterday I was asked to run a group therapy session on identity using an art based approach. The clients were a group of people coming to our trauma treatment program and I had not worked with them before. I was told that the group were a bit flat and struggling in the morning and later that day I discovered that the group had previously been having difficulty feeling connected.
Here is a brief outline of the group process I used.
Selecting images
I asked participants to select postcard images (free ones collected from cafes over the years) to describe aspects of themselves which were nothing to do with the experiences or struggles that brought them to our program. Naturally that was difficult as they were feeling overwhelmed by the problems they face, I let them know that even one card that did not relate to problems would be a good job done.
Then I asked them to cluster the cards into groups that seemed to fit together and give each group a name. (This clustering and naming process is a standard MIECAT arts therapy process it helps people make sense of the images and reduce the information held in the cards down to its core message)
The interview process
Group members were instructed to listen to the interview and take down any words or statements that they heard coming out of the interviewees mouth, which stood out to them for any reason. (this is another wonderful MIECAT technique called Key Words. It can be utilised in numerous ways; in this instance, it is serving the purpose of helping the listeners stay focused and engaged and the words collected are essential in our witnessing process)
Facilitator I interviewed each person about the cards they had chosen for about ten minutes. I invited participants to speak of the cards that were not dominated by problems and listened intently for the slightest opportunity to enquire into storylines which would lead the conversation to areas of the participant’s values, skills, knowledge, meaning full relationships etcetera. (In Narrative Therapy these are sometimes called windows of opportunity)
Participants After each interview participants took note of any key words or statements that had strongly resonated with their own experience and then gave all the words they had recorded to the speaker. Participants received these key words with delight.
Key word poetic statements Once everyone had been interviewed I invited participants to pluck out the words and statements that held the most meaning to them from the key words they had been given. (picking out the key words from the key words) they then created poetic statements with the words which they shared with the group. (this is another tried and true MIECAT procedure which again brings the many words down to the essence of what is most important to the individual)
Double listening
Not surprisingly speaking about stories not dominated by problems was very difficult for all the group members on this occasion so I needed to listen intently employing what is sometimes called double listening. Double listening is when you are with one ear hearing the problem dominated story and with the other ear listening for implicit or explicit fragments of preferred identity stories for example values held, skills and knowledge acquired, capabilities developed, relationships of meaning etcetera. By remaining curious, paying close attention and asking skilful questions informed by my narrative therapy training to draw out these alternate stories our conversations took surprising and delightful paths.
Some of the noteworthy things we learned about the group members were: of a powerful and protective sense of wit, a capacity to make life enhancing choices at life’s important junctures, ability to step out of the critical mind whilst play music which might translate into other parts of life, a passion for art and activism, values of living life to its fullest and an emerging capacity for self-compassion.
The power of being witnessed.
Through these conversations the group learned a great deal about each other’s lives which had not previously been explored and participants expressed a new-found appreciation for their group members. The stories we heard in this group stand in stark contrast to the stories of childhood abuse, workplace bullying and injury, emotional suffering, and decreased functioning through which the group had previously known one another. Having your courage, humour, passion, values and capability witnessed by an audience and reflected to you in your own words or through visual image is a powerful tool in reclaiming your sense of self from the effects of traumatic experience or illness.
When the team leader met with the group at the end of the day he described participants as buzzing with excitement when he entered the room and the group reported feeling much more connected with one another than they previously had.
Possibilities to include further art making
There are numerous ways to include more art making into this exercise here are some I have included in the past.
Initial representation can be made in any arts modality.
Visual representation of the essence of the key words can made by interviewee.
Each audience member makes a response in arts modality inspired by the key words they have collected to give to the interviewee.
Audience members make a representation of how the interview might inspire them in their own lives.
A rough outline of Outsider witness process
One person is interviewed by a narrative therapist in front of an audience of one or more.
The audience is then interviewed and asked to reflect on the following.
Some aspect of the interviewees story that caught their attention.
What that aspect of the evoked for them in terms of the interviewees hopes, values ambitions and identity.
How this relates to their own experience.
Where they might have been moved to or how they might be inspired by the experience of listening to the interview.
The original interviewee then speaks about their experience of listening to the audience (the retelling)
If you would like to read more about the use of outsider witness practice in Narrative Therapy I recommend the following article it is readily available on the internet.
Outsider-witness practices: some answers to commonly asked questions”
Maggie Carey & Shona Russell






 RSS Feed
RSS Feed